Mantle cell lymphoma (MCL) is a chronically relapsing B cell lymphoproliferative malignancy characterized by translocation t(11;14)(q13;q32), cyclin D1 overexpression and significant chromosomal instability. One of the main hypotheses of MCL relapses is a clonal evolution driven by therapy selection of subpopulations carrying adverse genetic and epigenetic aberrations. Our previous whole exome sequencing analysis of 25 MCL tumors showed that the majority of the detected single-nucleotide variants and copy number variants (CNV) were already detectable at diagnosis. To further analyze the subclonal structure of MCL at diagnosis and clonal evolution at relapse, we implemented single cell RNA sequencing analysis of five patients with MCL at diagnosis and at the first clinical relapse after failure of standard immunochemotherapy. All analyzed patients achieved at least partial remission.
Fresh-frozen tumor cells were sorted to obtain Hoechst − CD45 + population which was processed using single cell 3′ protocol (10X Genomics). The libraries were paired-end sequenced on Novaseq 6000 (Illumina). The reads were aligned to GRCh38 human genome. The MCL cells were distinguished from the normal B cells based on of CCND1 expression and unsupervised clustering. CNVs were predicted using inferCNV package. These CNVs shared a high degree of similarity with the CNVs predicted using available exome sequencing data.
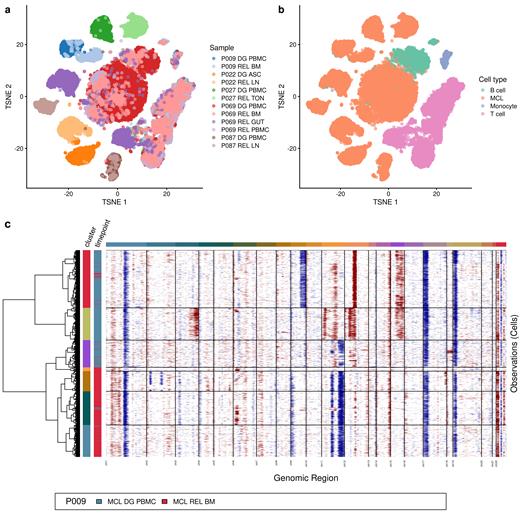
The t-SNE representation of the data clearly showed unique positions for the malignant lymphocytes obtained from each of the five analyzed patients ( Figure 1a). In contrast, non-malignant cells (T cells, B cells and monocytes) have grouped together irrespective of the patient or compartment of origin ( Figure 1b). These data suggest two conclusions. First, each patient's malignant cells have unique genetic background. Second, the impact of the microenvironment does not override the impact of the genetic makeup of the non-malignant cells. The data thus suggest comparability of the malignant cells obtained from different compartments.
Hierarchical clustering of the per-cell CNV profiles revealed subclonal heterogeneity of the MCL population in all analyzed compartments both at diagnosis and at relapse. In all analyzed patients the clustering identified several large subclones with significant differences (DG L) and at least one minor subclone (DG S) with significant similarities compared to the major clone detectable at relapse (R L). These data suggest that the majority of the diagnostic MCL cells (i.e., DG L clones) were indeed eliminated by therapy, which on clinical level corresponded to achieving remission. On the other hand, the data also suggest that MCL cells with CNV profiles highly similar to the major relapse clone (i.e., R L) were detectable already at diagnosis (i.e., DG S, Figure 1c).
To gain a better insight into the biology of the DG S clones with potential drug-resistant phenotype, we analyzed transcriptome differences between DG S and DG L clones. For each patient we identified different sets of significantly upregulated genes in DG S compared to DG L. These included genes coding for important cell surface molecules ( MARCKS, CD52, CD79A, LTB), regulators of cell motility and cytoskeleton dynamics ( STMN1, SWAP70, CFL1, TUBB, TUBA1B, TMSB4X), transcription factor PRDM2, energy metabolism proteins ( MT-ND4, MT-CO1, ATP5MG), protein degradation proteins ( UBA52, PSMC4, UFD1, UBE2L3) and others. Among these genes, significant upregulation of TMSB4X, SWAP70, HLA-A, TUBB4B, RPS26, UBA52, PSMB2, SNRPG, ARPC1B, ATP5MG was detected in three out of five patients. Many of these genes code for oncogenes involved in cell motility and aggressiveness.
To further characterize subclonal clusters in MCL population we used marker gene detection and subsequent gene set enrichment analysis, which identified cell adhesion molecules as major category upregulated in four out of five patients in clusters associated with relapse.
Our data shows the applicability of the single cell genomic approaches not only to analyze subclonal heterogeneity for the study of disease biology, but also to identify drug-resistant subclones at diagnosis, predict response to various types of therapies thereby enabling therapy personalization.
Acknowledgement: Supported by Grant Agency of the Czech Republic GA23-05474S and National Institute for Cancer Research (EXCELES) LX22NPO5102.
Disclosures
Klanova:Tubulis: Ended employment in the past 24 months. Trněný:Gilead Sciences, Takeda, BMS, F. Hoffmann-La Roche Ltd, Janssen, AbbVie: Other: Travel, Accommodation, Expenses; Janssen, Gilead Sciences, Takeda, BMS, Amgen, AbbVie, F. Hoffmann-La Roche Ltd, MorphoSys, Novartis: Honoraria; Takeda, BMS, Incyte, AbbVie, Amgen, F. Hoffmann-La Roche Ltd, Gilead Sciences, Janssen, MorphoSys, Novartis, Genmab, SOBI: Consultancy.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal